Your Mouth Matters – The Link Between Oral Health and Overall Health
Bleeding gums, a dull toothache, or morning breath that never seems to go away can feel like small annoyances. Many people shrug them off, assuming they are “just dental problems.” Yet research keeps pointing to a very real link between oral health and overall health, and that link is far stronger than most realize.
The mouth connects directly to the body’s major systems. It feeds into the digestive tract and shares space with the airway. It is home to millions of bacteria, some helpful and some harmful. When those harmful bacteria gain the upper hand, they do not always stay in the mouth. They can enter the bloodstream, spark inflammation, and place extra strain on the heart, lungs, brain, and more. This is the heart of the link between oral health and overall health.
At Toland Dental in Melbourne and West Melbourne, Florida, we see every day how problems like gum disease, dry mouth, and tooth loss tie into conditions such as heart disease, diabetes, sleep apnea, and even pregnancy complications—connections supported by research showing that oral health equals total health and quality of life. Many of these issues are preventable when people understand that their teeth and gums are part of their whole-body health, not separate from it.
In this guide, we walk through what science tells us about the link between oral health and overall health, how different conditions connect to the mouth, and what can be done at home and in the dental office to lower risk. The goal is not to scare anyone, but to replace worry with clear information. With the right knowledge and a caring dental team, it becomes much easier to protect the health of an entire family.
“You cannot be healthy without oral health.”
— U.S. Surgeon General
Key Takeaways
The link between oral health and overall health works in both directions. Problems in the mouth can strain the heart, lungs, blood sugar, and brain, and medical conditions can make gum disease and tooth decay harder to control. When one area improves, the other often improves too.
Gum disease, tooth infections, and heavy plaque growth raise inflammation in the body. That extra inflammation is tied to higher risks for heart disease, stroke, diabetes complications, breathing problems, pregnancy issues, and some cancers. Keeping gums healthy lowers this inflammatory burden and protects more than just teeth.
Preventive care is the foundation of both oral and overall wellness. Daily brushing, cleaning between teeth, healthy food choices, and avoiding tobacco all support the link between oral health and overall health in a positive way. Small daily habits add up over years.
Regular dental visits act as an early warning system for many conditions. Dentists can spot signs of diabetes, immune disorders, dry mouth from medications, sleep apnea concerns, and even oral cancer while they are still in early stages.
At Toland Dental, we combine family-friendly preventive dentistry, cosmetic care, restorative treatment, and sleep apnea services in one place. Our gentle, anxiety-aware approach helps children, adults, and seniors use the link between oral health and overall health to stay healthier and feel better at every age.
What Is The Link Between Oral Health And Overall Health?
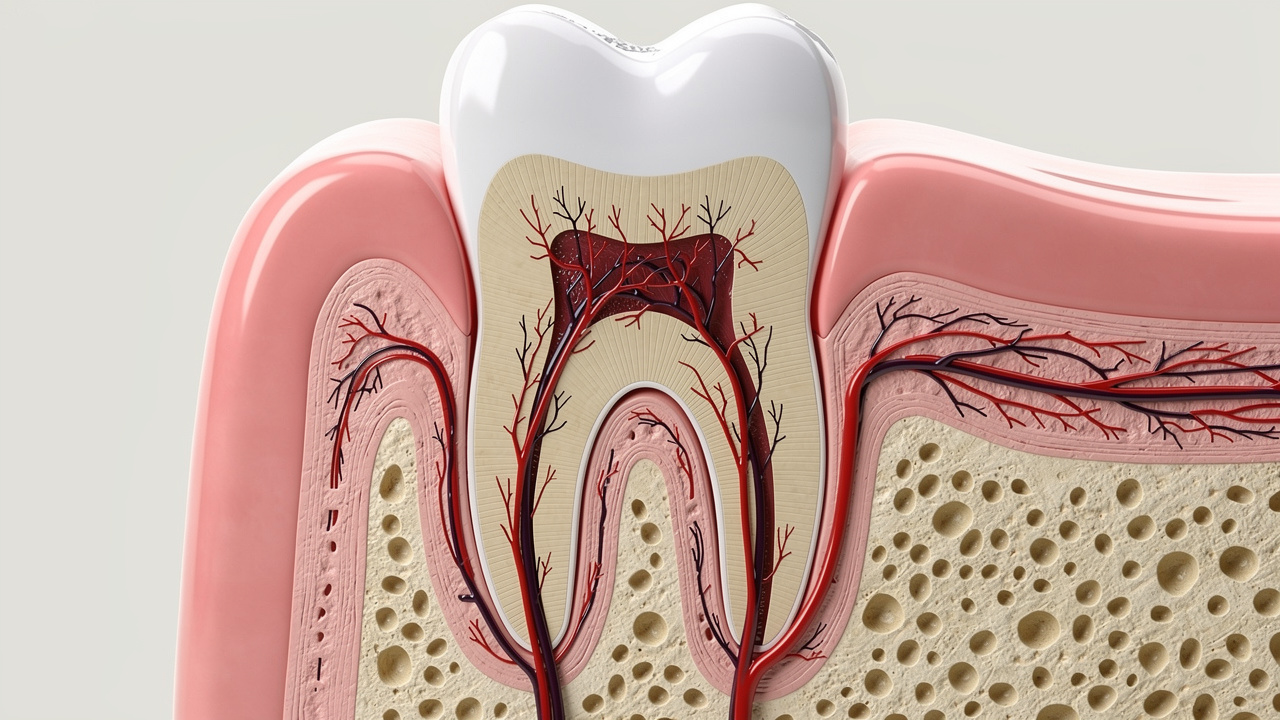
When most people think of oral health, they picture cavities and maybe a sore tooth now and then. In reality, oral health covers the gums, the bone around the teeth, the jaw joints, the muscles used to chew and speak, and the soft tissues that line the cheeks, lips, and tongue. All these structures sit at the entrance to the digestive and respiratory systems, where they play a direct role in total body health.
The mouth is crowded with bacteria. In a healthy state, these bacteria stay in balance, and the body’s defenses plus good home care keep them from causing trouble. When plaque builds up and gums become inflamed, that balance breaks down. Bacteria and their toxins can slip into the bloodstream through tiny breaks in swollen gum tissue. Once inside the circulation, they can travel to the heart, the brain, the lungs, and other organs.
Inflammation is a key part of the link between oral health and overall health. Gum disease is a chronic inflammatory infection. The body responds by sending out chemical signals and immune cells, which raises overall inflammatory levels. Over time, that ongoing inflammatory load is linked with damage to blood vessels, poorer blood sugar control, and greater strain on major organs.
The relationship also runs in the other direction. Conditions such as diabetes, autoimmune diseases, and dry mouth from medications can make it much easier for gum disease and tooth decay to develop. At Toland Dental, families often ask whether a problem in the mouth could be related to a problem somewhere else. The answer is often yes, and understanding this connection is the first step toward better health choices.
“Oral health is essential to general health and well-being.”
— American Dental Association
Your Mouth As A Gateway: Understanding The Biological Connection
The mouth is the front door to both the digestive tract and the airway. Food passes through the mouth, moves down the esophagus, and travels through the stomach and intestines. Air passes through the nose or mouth, down the throat, and into the lungs. This shared space means that anything living in the mouth has a direct path deeper into the body.
When gums are healthy and tight against the teeth, bacteria have a harder time crossing into the bloodstream. In gum disease, the gums pull away and form pockets around the teeth. These periodontal pockets trap food and bacteria. The lining of the pockets becomes thin, delicate, and inflamed, which makes it easier for bacteria and their toxins to slip into tiny blood vessels.
Once oral bacteria move into the bloodstream, they can attach to fatty deposits inside blood vessels, settle on damaged heart valves, or reach distant organs. The immune system reacts, sparking more inflammation. Over months and years, this constant low-level attack can wear down tissue far from the mouth.
Knowing that the mouth is such a key gateway can feel unsettling, but it is also empowering. When families understand this pathway, they can see how much difference simple steps like brushing, flossing, and regular dental cleanings can make for the body as a whole.
The Role Of Bacteria And Inflammation In Disease Development
Not all mouth bacteria are harmful. Many are part of a normal, healthy community that helps protect the teeth and gums. Problems start when sticky plaque is not removed and hard tartar forms along the gumline. This build-up gives harmful bacteria a safe place to grow and release toxins.
The first stage of this process is gingivitis, which causes red, swollen gums that bleed easily. If plaque and tartar stay in place, gingivitis can progress to periodontitis, a deeper infection that damages bone and ligament around the teeth. During this stage, the gums form pockets that harbor more aggressive bacteria.
These bacteria and the body’s response to them trigger inflammatory markers such as C-reactive protein and cytokines. These chemicals do not remain local. They circulate through the bloodstream and have been linked with heart disease, stroke, diabetes complications, and other systemic problems. Professional cleanings at Toland Dental break up these bacterial communities, smooth root surfaces, and help shut down this cycle of inflammation. With steady home care and routine visits, most people can keep these disease processes from taking hold.
How Does Poor Oral Health Affect Your Heart And Cardiovascular System?

Heart disease is still a leading cause of death in the United States, so any factor that adds risk deserves attention. Research over the last several decades shows a strong connection between moderate to severe gum disease and higher rates of heart attack and stroke. The link between oral health and overall health is very clear in this area.
When gums stay inflamed over long periods, bacteria enter the bloodstream again and again. Some of these bacteria can latch onto fatty deposits in the arterial walls. Others may trigger the body to create more of these deposits, known as plaque. In both cases, the arteries become narrower and stiffer, which limits blood flow to important organs.
Inflammation connects the link between oral health and overall health to the heart in another way. The same inflammatory chemicals that help fight gum infections can also damage the inner lining of blood vessels. This damage makes it easier for cholesterol and other fats to stick, which speeds the progress of atherosclerosis. In addition, oral bacteria have been found in the clots that cause some heart attacks and strokes.
There is also a relationship between poor oral health and endocarditis, a serious infection of the inner lining of the heart. While endocarditis is rare, it shows how far oral bacteria can travel when gum health breaks down. At Toland Dental, we review each patient’s medical history, especially any heart conditions, and work with cardiologists when needed so that preventive dental care supports cardiovascular wellness.
Understanding Atherosclerosis And Arterial Inflammation
Atherosclerosis means that arteries become hard, thick, and narrow because of fatty deposits along their walls. These deposits, called plaques, can limit blood flow or break apart and form clots. Either outcome raises the risk of heart attack and stroke.
Oral bacteria from diseased gums can move into the bloodstream and attach to these developing plaques. Once there, they stir up the immune system and trigger more inflammation. The immune cells that come to fight the bacteria can release substances that further damage the arterial wall and add to the plaque.
Over time, this inflammatory cycle makes the plaques larger and more fragile. Pieces can break off and travel to the heart or brain, blocking blood flow. While not every person with gum disease will develop heart disease, the link between oral health and overall health becomes very real for many. Regular cleanings, careful gum care, and early treatment of periodontal problems at Toland Dental help lower the inflammatory load on the arteries and support heart health.
Endocarditis: A Serious But Preventable Infection
Endocarditis is an infection of the inner lining of the heart chambers or valves. It can damage heart valves and, without fast treatment, can be life-threatening. One of the known sources of bacteria that cause endocarditis is the mouth, especially when gum disease or untreated tooth infections are present.
Bacteria from the mouth can enter the bloodstream during normal daily activities, such as chewing or brushing inflamed gums. In most healthy people, the immune system clears these bacteria quickly. In people with artificial heart valves, certain birth defects of the heart, or a history of endocarditis, the bacteria can stick to the heart lining and start an infection.
Symptoms may include fever, chills, fatigue, shortness of breath, and small spots on the skin or inside the mouth. People in higher-risk groups often receive antibiotics before some dental procedures to reduce this risk. At Toland Dental, we always ask about heart problems and communicate with cardiologists when needed. With good oral care, proper medical guidance, and gentle dental treatment, patients with heart conditions can stay safe and still receive the care their teeth and gums need.
Can Gum Disease Affect Blood Sugar And Diabetes Management?

The relationship between diabetes and gum disease is one of the clearest examples of the link between oral health and overall health. It works in both directions. People with diabetes are more likely to develop periodontitis, and people with periodontitis often have a harder time keeping blood sugar in a healthy range.
Gum disease is a chronic infection. Like any infection, it causes the body to release stress hormones and inflammatory chemicals. These substances can raise blood sugar and make cells less sensitive to insulin. For someone with diabetes, this can mean higher readings, more medication, and more risk for complications over time.
On the other side, high blood sugar weakens the immune system. It becomes harder for the body to fight oral bacteria, so gum infections can grow deeper and more stubborn. High sugar levels in saliva also feed harmful bacteria and lead to more plaque growth, which pushes the cycle along.
Research shows that when people with diabetes receive thorough periodontal treatment and then keep up with home care, their HbA1c levels often drop. At Toland Dental, we ask every diabetic patient about their blood sugar control, medications, and recent lab results, then design a gum care plan that supports their medical treatment. This might include more frequent cleanings, local antibiotic therapy for deep pockets, and close follow-up to keep inflammation as low as possible.
How Periodontal Disease Impacts Blood Glucose Control
When the gums are infected, the body reacts as it would to any ongoing infection. Hormones such as cortisol rise, and inflammatory cytokines circulate throughout the body. These chemicals can make it harder for insulin to move sugar from the blood into cells, a problem known as insulin resistance.
Higher insulin resistance means higher blood sugar levels, even if a person takes their medications correctly and follows their meal plan. Studies have found that people with moderate to severe gum disease often have higher HbA1c readings than people with healthy gums, even when other factors are similar. After deep cleaning and proper gum therapy, many see an improvement in those readings.
This shows the tight link between oral health and overall health for people with diabetes. Treating gum disease is not just about saving teeth. It also supports better blood sugar control and may lower the risk of eye, kidney, and nerve complications. At Toland Dental, we explain this connection clearly so that diabetic patients can see dental care as a key part of their diabetes plan.
Why Diabetics Are More Susceptible To Gum Disease
Diabetes affects the small blood vessels that supply the gums and bone around the teeth. Reduced blood flow makes it harder for the body to bring in infection-fighting cells and remove waste products. This slows healing and gives bacteria more time to cause damage.
High blood sugar also changes the way collagen, a key support fiber in gums and ligaments, breaks down and rebuilds. The tissues become more fragile and less able to repair everyday wear. Many people with diabetes also experience dry mouth, which lowers the protective power of saliva and encourages plaque build-up.
Because of these factors, even mild plaque build-up can trigger more severe gum responses in diabetic patients. That is why we often recommend that people with diabetes visit Toland Dental every three to four months for cleanings and gum checks. With careful home care, a low-sugar diet, and coordinated medical and dental follow-up, many diabetic patients can keep their gums healthy and protect their long-term health.
What Is The Connection Between Oral Health And Respiratory Illnesses?
The mouth sits right next to the airway, so it is not surprising that there is a strong link between oral health and overall health when it comes to breathing. Bacteria from the mouth can be drawn into the lungs, especially in people who have trouble swallowing, spend long periods in bed, or already have lung disease.
Research has connected poor oral hygiene and gum disease with higher rates of pneumonia, especially in hospitals and nursing homes. In these settings, patients may not clean their mouths well, and thick plaque layers become a reservoir for harmful bacteria. When those bacteria are inhaled, they can cause infection in the lungs.
People with chronic respiratory conditions such as COPD or asthma may also be affected. Their airways are already inflamed and sensitive. Adding more bacteria and inflammatory chemicals from the mouth can make breathing problems worse and increase flare-ups. Some inhaled medications can dry out the mouth, which raises the risk of cavities and gum disease, feeding the cycle.
At Toland Dental, we pay close attention to breathing issues and sleep concerns. Our work in sleep apnea and snoring therapy shows us every day how oral structures, airway health, and overall wellness fit together. By helping patients keep a clean, healthy mouth, we support better lung function and more restful sleep across generations.
Aspiration Of Oral Bacteria: The Pathway To Lung Infections
Aspiration means that material from the mouth or stomach enters the airway and lungs instead of going down the esophagus. This can happen in small amounts during sleep, especially in people who snore or have reflux, and in larger amounts in people who have swallowing problems or are very weak.
When plaque and tartar are heavy, the bacteria living there can be pulled into tiny droplets of saliva and then inhaled. Once in the lungs, these bacteria can settle in the air sacs and start an infection. In someone with a strong immune system and healthy lungs, the body often clears them. In older adults, hospital patients, or those with chronic lung disease, the bacteria can lead to pneumonia.
Good oral hygiene reduces the number of harmful bacteria available for aspiration. Regular brushing, cleaning between teeth, and professional cleanings at Toland Dental lower the bacterial load so that even if aspiration happens, there is less risk that it will cause serious lung problems.
Chronic Respiratory Conditions And Oral Health Maintenance
For people living with COPD, asthma, or other long-term breathing disorders, mouth care becomes even more important. These conditions are often managed with inhaled medications that can dry the mouth or leave residue on teeth and gums. Dryness lowers saliva’s natural cleaning action and can cause more cavities and gum irritation.
To make daily care easier, it often helps to:
Rinse with water after using inhalers.
Brush gently twice a day with a soft toothbrush.
Clean between teeth daily with floss, picks, or a water flosser.
Schedule shorter, more frequent dental visits if breathing is limited.
The constant effort of breathing can also make long dental visits uncomfortable. At Toland Dental, we schedule flexible appointments when needed and offer relaxing positions that support easy breathing. Regular dental checkups allow us to watch for early signs of infection, dry mouth damage, or gum disease so that we can step in quickly. By treating oral problems early, we help reduce extra strain on the lungs and support better day-to-day comfort.
How Does Oral Health Impact Pregnancy And Birth Outcomes?

Pregnancy affects the whole body, including the mouth. Hormone shifts can make gums more reactive to plaque, leading to tender, swollen tissue that bleeds easily. Many expectant mothers notice “pregnancy gingivitis,” small growths on the gums, or changes in breath. These changes connect to a wider link between oral health and overall health for both mother and baby.
Studies show that mothers with untreated periodontitis have higher rates of preterm birth and low birth weight, with research documenting how oral health educational interventions during pregnancy can improve both maternal oral health and birth outcomes. The exact reasons are still under study, but oral bacteria and inflammation seem to play a role. Bacteria from deep gum pockets may enter the bloodstream and reach the placenta or amniotic fluid. Once there, they can trigger inflammatory chemicals that may start labor too early.
Morning sickness, food cravings, and frequent snacking can also affect teeth. Stomach acid from vomiting can erode enamel, and sugary snacks feed cavity-causing bacteria. If dental care is delayed because of worry about safety during pregnancy, these problems can grow larger and harder to treat later.
At Toland Dental, we see pregnancy as a key time to support the link between oral health and overall health. We work closely with expectant mothers to manage gum health, control decay, and provide calm, gentle care in every trimester. This helps protect the mother’s comfort and may also support better birth outcomes.
The Mechanisms Linking Gum Disease To Preterm Birth
Researchers believe that oral bacteria can move from inflamed gums into the bloodstream and then reach the uterus and placenta. Once they arrive, the immune system reacts by releasing inflammatory mediators such as prostaglandins. These substances are the same ones that help start labor at the proper time near the end of pregnancy.
If prostaglandin levels rise too early, the body may begin labor before the baby is fully ready. Inflammation around the placenta can also affect how well it works, limiting nutrients and oxygen to the baby and raising the chance of low birth weight. Studies show that women with advanced periodontitis have a higher risk of these problems compared with women who have healthy gums.
The good news is that treating gum disease before or during pregnancy appears safe and helpful. Professional cleanings, careful root planing when needed, and good home care can lower bacterial levels and inflammation. At Toland Dental, we encourage women who plan to become pregnant to have a full dental checkup first, so that any gum issues can be handled early.
Safe Dental Care During Pregnancy: What Expectant Mothers Need To Know
Many pregnant women worry that dental care might harm their baby, so they avoid visits until after delivery. In fact, routine dental care and needed treatment are considered safe during pregnancy and are strongly recommended. Waiting can allow infections to spread, which is riskier for both mother and child.
Key points for pregnant patients include:
The second trimester is often the most comfortable time for dental visits.
Urgent dental care can be provided in any trimester when needed.
Dental x-rays with proper shielding use very low radiation and are safe when limited to what is necessary.
Local anesthetics used by dentists have been widely studied and are safe for pregnant patients.
Managing pregnancy gingivitis with gentle cleanings, soft brushing, and flossing is important for comfort and health. Rinsing with water after morning sickness helps clear acid and protect enamel. At Toland Dental, we invite expectant mothers to share their pregnancy status, due date, and any medical recommendations so that we can plan the safest and most comfortable care for them.
Is There A Link Between Oral Health And Cognitive Function?
Many people are surprised to learn that there may be a link between oral health and overall health that reaches all the way to the brain. Studies have found connections between long-term gum disease and a higher risk of memory problems, including dementia and Alzheimer’s disease.
One theory is that bacteria from chronic periodontitis can enter the bloodstream or travel along nerve pathways to the brain. Once there, they may trigger inflammation that harms brain cells. Over time, this repeated low-level insult could play a part in the slow loss of memory and thinking ability.
A specific gum disease bacterium, Porphyromonas gingivalis, has been found in the brain tissue of some people with Alzheimer’s disease. Toxins released by this bacterium seem able to damage nerve cells in lab settings. While these studies do not prove that gum disease causes dementia, they do support a strong link between oral health and overall health in this area.
The relationship is also bidirectional. As memory and daily function decline, personal care routines such as brushing and flossing become harder to manage. This leads to more plaque, more cavities, and more infections, which may increase inflammation in the body. At Toland Dental, we work with patients, families, and caregivers to keep oral care simple and consistent for older adults.
How Oral Bacteria May Reach The Brain
Oral bacteria can move beyond the mouth in several ways. The most common pathway is through the bloodstream. When gums are inflamed and bleed easily, bacteria have a clear opening into small blood vessels. From there, they can circulate and, in some cases, cross the blood-brain barrier, the protective lining around the brain.
Another possible route is through cranial nerves that connect the mouth and face to the brain. Some studies suggest that bacteria may travel along these nerve fibers over time. Researchers have discovered DNA from gum disease bacteria and their toxins in the brain tissue of people with Alzheimer’s, which fits this theory.
These bacteria and toxins can trigger inflammation and may directly injure brain cells. While the science is still developing, the pattern supports the idea that protecting gum health may also help protect brain health. Lifelong attention to oral hygiene and regular visits to a dentist such as Toland Dental give people the best chance to lower these potential risks.
Maintaining Oral Health To Support Brain Health As We Age
As people age, arthritis, vision changes, and memory loss can make daily oral care more challenging. Yet this is the time when the link between oral health and overall health becomes especially important.
Helpful adjustments include:
Using electric toothbrushes with larger handles for better grip.
Choosing floss holders or water flossers to clean between teeth.
Setting reminders or routines for brushing twice a day.
Involving caregivers for step-by-step prompts or hands-on help.
Regular professional care also becomes more important with age. At Toland Dental, we schedule gentle, unhurried visits for older adults, check dentures and implants carefully, and look for early signs of infection or dry mouth. By supporting oral health in later life, we aim to support comfort, confidence, and possibly better brain function as well.
Can Poor Oral Health Increase Cancer Risk?
Chronic inflammation is a known risk factor for many types of cancer, and gum disease is a major source of chronic inflammation in the body. This makes the link between oral health and overall health very relevant when talking about cancer risk.
Studies have found that people with long-term periodontitis may have a higher chance of developing cancers of the mouth, throat, and esophagus. There are also reported links with cancers of the pancreas, lung, and some other organs. While many factors play into cancer risk, the ongoing inflammation and bacterial exposure from diseased gums seem to add to the burden.
Oral cancer itself is a serious concern. It often starts quietly, with a small sore, a red or white patch, or a lump that does not hurt. Risk is higher in people who use tobacco, drink heavily, or have certain strains of HPV. Regular oral cancer screenings during dental checkups can spot these changes early, when treatment works best.
At Toland Dental, we include a careful oral cancer screening as part of every comprehensive exam. We look at the tongue, cheeks, lips, roof and floor of the mouth, and the back of the throat. This is one more way that a focus on the link between oral health and overall health can protect long-term wellness.
Understanding The Inflammation–Cancer Connection
Inflammation is the body’s way of responding to injury or infection. In the short term, it helps with healing. When inflammation lasts for months or years, it can start to damage normal cells. The chemicals released during chronic inflammation can create oxidative stress, which harms DNA.
Damaged DNA can lead to mistakes when cells divide. Over time, these mistakes can build up and raise the chance that a cell will grow out of control, which is the basis of cancer. In the mouth, long-standing gum disease keeps tissues bathed in inflammatory chemicals and bacterial toxins.
Because of this, controlling gum inflammation is an important step for lowering cancer risk. Regular cleanings, good home care, and early treatment of gum problems reduce the constant irritation that keeps inflammation going. At Toland Dental, we view periodontal care as a key part of long-term cancer prevention efforts.
Oral Cancer Screening: Early Detection Saves Lives
During an oral cancer screening, we visually and gently examine all the soft tissues in and around the mouth. We look for sores that do not heal, patches that are white or red, thickened areas, or lumps. We also feel along the neck and jaw for enlarged lymph nodes or other unusual changes.
Warning signs patients can watch for between visits include:
Mouth sores that last more than two weeks.
Difficulty swallowing or a feeling of something caught in the throat.
Changes in the way teeth fit together.
Persistent hoarseness or numbness in the mouth or lips.
Risk increases with tobacco use, heavy alcohol use, and certain HPV infections, but oral cancer can appear in people without these factors as well. Cancers found early have a much higher chance of successful treatment. Screenings are quick, painless, and included in routine exams at Toland Dental. By staying alert to small changes, both at home and in the dental office, patients give themselves the best chance of early detection.
How Do Systemic Health Conditions Affect Your Mouth?
The link between oral health and overall health is not just about the mouth harming the body. Many systemic conditions show their first signs in the mouth or make oral health harder to maintain. Understanding this two-way street helps patients and providers plan better care.
Autoimmune diseases, for example, can cause painful mouth sores, dry mouth, or gum problems. Conditions such as Sjögren’s syndrome, lupus, and rheumatoid arthritis often bring oral symptoms that affect comfort and daily function. Medications used to treat these diseases may also affect saliva flow or increase infection risk.
HIV and other conditions that weaken the immune system can lead to frequent oral infections, such as thrush or viral lesions. Eating disorders can erode enamel and change the look of the gums and soft tissues. Many common medications, including some for blood pressure, mood, and allergies, can dry the mouth and raise cavity risk.
At Toland Dental, we ask detailed medical questions because they matter for the mouth. We frequently coordinate with physicians, share findings, and adjust dental plans to match each person’s health status. For medically complex patients, a gentle, informed dental home can make a big difference in comfort and safety.
Autoimmune Conditions And Oral Health
Autoimmune diseases occur when the immune system mistakenly attacks the body’s own tissues. In Sjögren’s syndrome, the glands that make saliva are damaged, which leads to severe dry mouth. Without enough saliva, food particles and acids are not washed away, so cavities and gum disease can progress quickly.
Rheumatoid arthritis shares inflammatory features with periodontitis. People with this condition have higher rates of gum disease, and their hand pain can make brushing and flossing difficult. Lupus can cause mouth ulcers, dry mouth, and changes in the appearance of the lips and inner cheeks.
Immunosuppressive medications used to manage these diseases can also increase the risk of oral infections. At Toland Dental, we work with autoimmune patients to create a simple, realistic home care plan, often with aids such as electric toothbrushes or water flossers. We recommend more frequent professional cleanings and monitor carefully for any early signs of infection or tissue changes.
HIV/AIDS And Oral Manifestations
HIV attacks the immune system, which leaves the body more open to infections, including those in the mouth. One common oral problem is candidiasis, or thrush, which appears as white, creamy patches that can be wiped off to reveal a raw surface underneath. Viral infections such as oral hairy leukoplakia, which shows as white patches on the side of the tongue, and Kaposi’s sarcoma, a type of cancer that can appear as dark spots on the palate, are also more common.
People living with HIV may experience more severe gum disease, with faster bone loss and deeper pockets. The pattern and severity of these oral findings can help medical teams understand how far the disease has progressed and how well treatments are working.
At Toland Dental, we follow strict infection control standards for every patient and offer confidential, respectful care. We encourage patients with HIV to share their status and medications so that we can adjust treatment plans, choose safe medications, and schedule visits in a way that supports their overall health.
What Role Does Saliva Play In Protecting Overall Health?
Saliva does far more than keep the mouth moist. It is an active part of the body’s defense system and a key player in the link between oral health and overall health. When saliva flow drops, problems can spread quickly from the mouth to the rest of the body.
Saliva contains minerals such as calcium and phosphate that help repair tiny areas of enamel damage before they turn into full cavities. It also neutralizes acids produced by bacteria after meals, which protects both teeth and the delicate tissues in the mouth. Natural antimicrobial substances in saliva slow the growth of harmful bacteria and fungi.
Beyond oral protection, saliva starts the digestive process by helping break down food and making it easier to swallow. Smooth swallowing is important for airway safety, because it keeps food and liquids out of the lungs. Dry mouth can lead to swallowing problems, soreness, and changes in taste, which may cause people to avoid certain foods and harm their nutrition.
Many medications, including some used for blood pressure, depression, allergies, and pain, can reduce saliva flow. Medical treatments such as radiation to the head and neck can damage salivary glands. At Toland Dental, we review medication lists carefully and help patients manage dry mouth so that the link between oral health and overall health stays positive, not harmful.
Medications That Cause Dry Mouth And How To Manage It
Several common types of medicine can reduce saliva. These include many antidepressants, anti-anxiety drugs, antihistamines, some blood pressure pills, diuretics, and certain pain medications. Cancer treatments that involve radiation to the face or neck can also weaken saliva glands.
When saliva falls, cavity and gum disease risk rises sharply. Without saliva to wash away food and neutralize acids, bacteria thrive and attack enamel and gum tissue. People may notice a sticky feeling in the mouth, trouble speaking clearly, or a burning sensation on the tongue.
Management starts with:
Sipping water often throughout the day.
Avoiding sugary drinks that feed bacteria.
Using sugar-free gum or lozenges to stimulate saliva.
Trying saliva substitute gels or sprays if recommended.
Using a humidifier at night to keep the mouth from drying out.
At Toland Dental, we often recommend prescription-strength fluoride toothpaste or in-office fluoride treatments for patients with chronic dry mouth, along with more frequent checkups. We always remind patients not to stop prescribed medications without talking with their physician.
Saliva As A Diagnostic Tool: The Future Of Health Monitoring
Saliva contains traces of many substances that reflect what is happening in the body. These include hormones, antibodies, genetic material from viruses and bacteria, and by-products of medications. Because of this, saliva is becoming an exciting tool for health monitoring.
Researchers are developing saliva tests that may detect conditions such as diabetes, certain cancers, hormone imbalances, and viral infections. Compared with blood tests, saliva tests are simple, painless, and easy to repeat. This could make regular health screening more comfortable and accessible for many people.
The growing use of saliva in diagnostics highlights the deep link between oral health and overall health. As these tests become more common, dental offices may play an even bigger role in early disease detection. Practices like Toland Dental are watching these developments closely so we can offer patients the benefits of this new technology when it becomes widely available.
How Can You Protect Both Your Oral Health And Overall Health?
The good news in all of this is that daily habits and regular dental care can greatly improve the link between oral health and overall health, as confirmed by a qualitative research study exploring how patients understand and act on the connection between their oral and systemic health. Protecting the mouth often protects the body, and small changes can have large effects over time.
A strong home routine is the starting point. Brushing, cleaning between teeth, and caring for the tongue and gums remove the bacteria that drive inflammation. Pairing this with a balanced diet low in added sugar and high in fruits, vegetables, and lean proteins supports both teeth and body.
Lifestyle choices matter as well. Tobacco products dramatically raise the risk of gum disease, tooth loss, and many cancers. High stress levels can lead to teeth grinding and make inflammation worse. Adequate sleep, stress management, and, when needed, sleep apnea treatment all play into the broader picture of health.
Professional care adds another layer of protection. At Toland Dental, we provide preventive cleanings, thorough exams, sleep apnea evaluation, restorative dentistry, dental implants, and cosmetic options such as KöR Whitening in a calm, family-centered setting. This full approach allows us to support families at every stage, from a child’s first cleaning to complex care for seniors, always with an eye on the link between oral health and overall health.
Essential Daily Oral Hygiene Practices

Effective brushing is the base of a healthy mouth. We recommend brushing at least twice a day for two full minutes with a soft-bristled toothbrush. Holding the brush at a forty-five degree angle toward the gums and using short, gentle strokes helps clean both teeth and gumline without causing damage.
To build a strong routine:
Use fluoride toothpaste to strengthen enamel.
Brush all tooth surfaces, including the backs of the front teeth.
Clean between teeth once a day with floss, floss picks, interdental brushes, or a water flosser.
Gently brush or scrape the tongue to reduce bacteria and improve breath.
Replace toothbrushes every three to four months, or sooner if bristles fray.
An alcohol-free antibacterial mouthwash can also lower bacterial levels and freshen breath. At Toland Dental, we show children, adults, and seniors simple techniques and tools, and we correct common mistakes we see, such as brushing too hard or skipping the back teeth.
The Importance Of Regular Professional Dental Care
Even with excellent home care, some plaque hardens into tartar that only dental tools can remove. Professional cleanings clear this build-up, smooth root surfaces, and polish away stains. During a comprehensive exam, we:
Check teeth for decay and cracks.
Measure gum depth and assess gum health.
Screen for oral cancer.
Review how the bite and jaw joints are working.
Discuss any signs of grinding, clenching, or sleep-related issues.
The right visit schedule depends on each person’s health status. Many people do well with visits every six months. Those with gum disease, diabetes, dry mouth, or a history of heavy tartar may need to come every three to four months. Early detection at these visits allows us to treat small problems before they become painful or expensive.
We know that fear, cost, and busy schedules can keep people away from the dentist. At Toland Dental, we focus on anxiety-aware care, clear communication, and family-friendly scheduling. We offer advanced technology and comfort touches to make visits as easy as possible. For patients with medical conditions, we coordinate with physicians to support safe, integrated care. Bringing the whole family to one trusted dental home makes it much simpler to keep the link between oral health and overall health working in everyone’s favor.
Conclusion
The science is clear. The mouth is not separate from the rest of the body. The strong link between oral health and overall health runs through the heart, lungs, blood sugar, pregnancy, brain function, and even cancer risk. Gum disease, untreated tooth infections, and dry mouth do more than cause pain or bad breath. They add to the body’s inflammatory load and can strain major organs over time.
The hopeful side of this story is that simple, steady care makes a real difference. Brushing, cleaning between teeth, eating well, avoiding tobacco, and keeping up with regular dental visits lower harmful bacteria and inflammation. In turn, this supports healthier arteries, better blood sugar control, easier breathing, safer pregnancies, and more comfortable aging. The relationship is bidirectional, so improvements in medical conditions can also make it easier to maintain a healthy mouth.
At Toland Dental, we see our role as partners in whole-body wellness. We welcome families, anxious patients, seniors, and those with complex medical histories into a calm, caring environment. From preventive cleanings and oral cancer screenings to sleep apnea treatment, dental implants, and KöR Whitening, we structure our care around the link between oral health and overall health.
Taking care of the mouth is one of the most practical ways to take care of the entire body. For anyone in Melbourne or West Melbourne, Florida, ready to protect their smile and their health, we invite you to contact Toland Dental. We would be honored to treat you like family and help keep every part of you as healthy as your smile.
Frequently Asked Questions (FAQs)
How Often Should I Visit The Dentist If I Have A Chronic Health Condition Like Diabetes Or Heart Disease?
Most people with conditions such as diabetes or heart disease benefit from cleanings and checkups every three to four months. These visits help control gum inflammation, which can affect blood sugar and heart strain. Regular exams also allow the dental and medical teams to share information. At Toland Dental, we adjust visit frequency based on each person’s health, medications, and risk, and we encourage open conversation about any changes in your medical care.
Can Gum Disease Really Cause A Heart Attack?
Gum disease does not act like a switch that directly causes a heart attack, but it raises the risk in a meaningful way. Bacteria from inflamed gums can enter the bloodstream, attach to artery walls, and trigger inflammation that supports plaque growth and clot formation. Studies show a clear connection between serious gum disease and higher rates of heart attack and stroke. Keeping gums healthy with good home care and regular visits to Toland Dental helps lower this added heart risk.
Is It Safe To Get Dental Work Done While Pregnant?
Yes, dental care is safe and recommended during pregnancy. The second trimester is often the most comfortable time for treatment, but urgent care can be managed at any stage. Delaying needed treatment can allow infections to spread, which is more dangerous for mother and baby. Dental x-rays with proper shielding and standard local anesthetics are considered safe. At Toland Dental, we work closely with expectant mothers and their doctors to choose the right timing and approach for each visit.
What Are The First Signs That My Oral Health Might Be Affecting My Overall Health?
Warning signs include gums that bleed easily, persistent bad breath, loose teeth, or mouth sores that do not heal within two weeks. Some people also notice trouble chewing, changes in taste, or repeated mouth infections. Systemic symptoms such as recurring low-grade fevers or swallowing problems can sometimes have an oral source. Because many connections are silent in early stages, regular exams matter a lot. If you notice any of these issues, schedule a visit at Toland Dental so we can check your mouth and guide next steps.
Can Improving My Oral Health Actually Help Me Manage My Diabetes Better?
Yes, research supports that better oral health can support better diabetes control. Treating gum disease lowers inflammation and infection, which can improve insulin sensitivity and reduce blood sugar levels. Many studies show that patients have lower HbA1c readings after thorough periodontal treatment and follow-up care. This can also reduce the risk of other diabetes-related problems over time. At Toland Dental, we work closely with diabetic patients to design gum care plans that support their medical treatment and long-term health goals.


